Climate Change and Children’s Health

Children, including adolescents under the age of 18, are often more vulnerable than the general population to the health impacts of climate change because:
- Children’s bodies are developing physically, which can make them more vulnerable to climate-related hazards like heat and poor air quality. They also breathe at a faster rate, increasing their exposure to dangerous air pollutants.1
- Children tend to spend more time outdoors than adults, increasing their exposure to heat and cold, rain and snow, outdoor allergens, and insect bites.2
- Children drink more water than adults per pound of body weight.3 They swallow about twice as much water as adults while swimming. This can increase their exposure to certain contaminants in recreational waters and the risk of developing gastrointestinal or other illnesses.4
- Children are developing emotionally, as their brains continue to grow throughout adolescence. Children can experience mental health impacts from major storms, fires, and other extreme events that are expected to increase with a changing climate. They also can suffer from other changes, such as having to move due to climate threats.
- Young children depend on adults for their safety and well-being. This dependence can put children at greater risk during extreme events. For example, without adult help, children may not be able to keep their heads above floodwaters or get to safety during a storm.5
Photo caption endnote:6
On this page:
- Key Threats to Children’s Health
- What You Can Do
- Investigate Other Populations At Risk
- Related Resources
- Endnotes
Key Threats to Children’s Health
A number of climate-related hazards threaten the health of children in the United States. Below are examples of the potential health impacts of these hazards.
- Respiratory Illnesses
- Heat Illnesses
- Water-Related Illnesses
- Insect- and Tick-Related Diseases
- Food System Impacts
- Mental Health Effects

Respiratory Illnesses
Climate change has the potential to increase outdoor air pollutants, such as dust from droughts, wildfire smoke, and ground-level ozone. Ground-level ozone and particulate matter are associated with increases in asthma and other respiratory conditions in children.10, 11 Climate change can also increase pollen and prolong the allergy season. Higher outdoor temperatures can lead to children spending more time indoors, where they can be exposed to indoor pollutants, such as tobacco smoke and mold.
Photo caption endnote:12
Heat Illnesses
Extreme heat events are expected to last longer and become more frequent and intense as the climate changes.13 Heat illnesses can occur when a person is exposed to high temperatures and their body cannot cool down. Increases in average and extreme temperatures are expected to lead to more heat illnesses and deaths among vulnerable groups, including children.14 Heat can affect children who spend time outdoors playing and exercising.

Young athletes are at particular risk of heat stroke and heat illnesses.15 Children who live in homes without air conditioning are also at risk. Young children and infants are particularly vulnerable to heat-related illnesses and death, as their bodies are less able to adapt to heat.16
Photo caption endnote:17
Water-Related Illnesses
Runoff from more frequent and intense rains, flooding, and coastal storms can introduce more pollutants and disease-carrying organisms into water bodies where children swim and play or that communities use as drinking water supplies.18
These contaminants can impact drinking water supplies and recreational waters.19 Untreated, contaminated water can cause gastrointestinal illnesses for any individual drinking or coming into contact with it;20 however, children have a higher risk of gastrointestinal illness if they come in contact with contaminated water than adults.21, 22

Increasing water temperatures associated with climate change can also encourage the growth of bacteria and harmful algae in coastal waters.23 This can lead to harmful algal blooms, which can make people sick if they swim or play near them.24 Because of the ways children tend to behave in water, they are at greater risk for getting sick compared to adults.25 In some areas, rising air and water temperatures will also extend the swimming season, increasing children’s risks of getting gastrointestinal and other water-related diseases, as well as eye and ear infections.
Photo caption endnote:26
When children are also part of other groups vulnerable to climate change, this compound effect can increase their health risks. For instance, Native American/Alaska Native infants are hospitalized more for diarrheal disease than infants in the general U.S. population—often due to a lack of safe and reliable drinking water.7 Extreme rainfall and warmer temperatures, which have been linked to bacterial contamination of drinking water, are expected to further impact tribal water supplies.8 In addition, children in low-income households and non-white children are more likely to be exposed to extreme heat and air pollution. They are also less able to escape from extreme weather events.9
Insect- and Tick-Related Diseases
Climate change is expanding the habitat ranges and length of time when insects and ticks are common.27 In some regions, that results in a northward expansion of where ticks may live; while other areas could also see ticks active for longer periods throughout the year.28 Warmer temperatures associated with climate change can also increase mosquito development and biting rates, while increased rainfall can create breeding sites for mosquitos.29
Because children spend a lot of time outdoors, they are vulnerable to insect and tick bites that can cause illnesses like West Nile virus and Lyme disease. In rare cases, West Nile virus can lead to serious or fatal sickness.30 Separately, studies show that children between the ages of 5 and 9 report a higher frequency of Lyme disease compared to most other age groups.31 Lyme disease can cause chronic pain and neurological problems if not treated early.32
Food System Impacts
Proper nutrition is essential for children’s physical and mental growth. Extreme events, such as wildfires, floods, heat waves, and droughts may disrupt food production and distribution, increase costs, and limit availability. These impacts could make it harder for children to get healthy food.33 Diseases, pests, and water shortages can also affect crop productivity and quality.
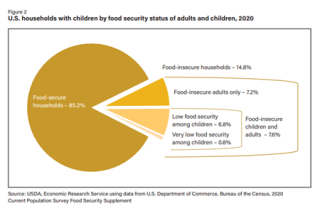
Most U.S. households are currently food secure. This means they have consistent, dependable access to enough food for active, healthy living. But millions of households with children experience food insecurity at times during the year. This means their access to adequate food is limited by a lack of money and other resources.34
Climate change may affect certain disease-causing organisms in the food chain.35 For instance, Escherichia coli (E. coli) could increase with a warmer and more humid climate.36 These climate changes, combined with other social and economic factors, may increase children’s vulnerability to some food-related illnesses. For example, children are more prone to severe illness or complications from E. coli infections.37
Photo caption endnote:38
Mental Health Effects
Children who go through a natural disaster or extreme weather event may have anxiety, depression, trouble sleeping, phobias, and post-traumatic stress.39 Children’s ability to cope with these events depends on many factors, including their living situation and support systems. There may be a perception that children are resilient to traumatic events. However, mental health impacts may last into adulthood, especially if left untreated.40
Parents, caregivers, coaches, and school administrators can take steps to reduce the health impacts of climate change on children. Consider the following action items:
- When temperatures soar, keep kids cool and encourage them to drink enough water. Watch for signs of dehydration or overheating. Offer sips of water often and find places to cool off. Have children exercise earlier in the day when it is cooler outside. Never leave children in a parked car. Wear sunscreen when outdoors.
- Check the Air Quality Index and pollen counts on your local weather reports. Also, pay attention to wildfire, smoke, and ash warnings. When the air quality is poor, consider limiting children’s time outdoors. Have children avoid playing in high-traffic areas.
- Protect children from indoor air pollution. Also consider a portable air cleaner or high-efficiency air filter to help improve your air quality indoors.
- Prevent mosquito bites. Clean up standing water where mosquitos like to reproduce.
- Prevent tick bites. Be aware of where ticks live. Have children wear long-sleeved shirts and long pants. Check children for ticks after they have been outdoors, especially during warmer months and when they have been in wooded or grassy areas.
- Choose the right insect repellent for your needs and use it according to the directions on the label. Do not allow children to apply insect repellent themselves. Instead, apply repellent for them, while taking care not to get any on their hands.
- Keep kids safe during and after an extreme weather event. Make sure your family has an evacuation or safety plan if you live in an area prone to severe weather. After a flood, watch for signs of mold and be sure to clean and dry affected areas. Focus on providing your children access to clean potable water, and avoid having them wade in floodwaters or be exposed to debris from disasters. If children are exposed to storms or floods, watch for diarrhea symptoms. Don’t allow children to participate in disaster cleanup to avoid exposing them to toxic materials which are often found in debris.
- Talk to your pediatrician if you think your child’s health, including their mental well-being, has been affected by climate change.
Related Resources
EPA resources:
Other resources:
Endnotes
1 Gamble, J.L., et al. (2016). Ch. 9: Populations of concern. In: The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 255.
2 Ibid, pp. 255–256.
3 Ibid, p. 255.
4 Ibid, p. 256.
5 Bell, J.E., et al. (2016). Ch. 4: Impacts of extreme events on human health. In: The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 108.
6 Trtanj, J., et al. (2016). Ch. 6: Water-related illness. In: The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 159.
7 Gamble, J.L., et al. (2016). Ch. 9: Populations of concern. In: The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 254.
8 Ibid, p. 256.
9 Ibid, p. 255.
10 Ebi, K.L., et al. (2018). Human health. In: Impacts, risks, and adaptation in the United States: Fourth national climate assessment, volume II. U.S. Global Change Research Program, Washington, DC, p. 544.
11 Gamble, J.L., et al. (2016). Ch. 9: Populations of concern. In: The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 256.
12 Centers for Disease Control and Prevention (CDC). (2021). Most recent national asthma data. Retrieved 3/11/2022.
13 Sarofim, M.C., et al. (2016). Ch. 2: Temperature-related death and illness. The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 51.
14 Crimmins, A., et al. (2016). Executive summary. In: The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 6.
15 Gamble, J.L., et al. (2016). Ch. 9: Populations of concern. In: The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 255.
16 Smith, K.R., et al. (2014). Human health: impacts, adaptation, and co-benefits. In: Climate change 2014: Impacts, adaptation, and vulnerability. Part A: Global and sectoral aspects. Contribution of working group II to the fifth assessment report of the intergovernmental panel on climate change. Cambridge University Press, Cambridge, United Kingdom and New York, NY, p. 717.
17 Gamble, J.L., et al. (2016). Ch. 9: Populations of concern. In: The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 255.
18 Lall, U., et al. (2018). Water. In: Impacts, risks, and adaptation in the United States: Fourth national climate assessment, volume II. U.S. Global Change Research Program, Washington, DC, p. 170.
19 Trtanj, J., et al. (2016). Ch. 6: Climate impacts on water-related illness. The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 161.
20 Ibid, p. 164.
21 Ibid, p. 170.
22 Ibid, p. 170.
23 Ibid, p. 158.
24 U.S. Environmental Protection Agency (EPA). (N.D.). Harmful algal blooms and drinking water. Washington, D.C., EPA: 810-F-16-006. Retrieved 3/11/2022.
25 Trtanj, J., et al. (2016). Ch. 6: Climate impacts on water-related illness. The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 170.
26 Gamble, J.L., et al. (2016). Ch. 9: Populations of concern. In: The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 256.
27 Beard, C.B., et al. (2016). Ch. 5: Vector-borne diseases. The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 142.
28 Ibid, p. 144.
29 Ibid, pp. 141–142.
30 Centers for Disease Control and Prevention (CDC). (2024). West Nile: symptoms, diagnosis, & treatment. Retrieved 7/22/2024.
31 Beard, C.B., et al. (2016). Ch. 5: Vector-borne diseases. The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 142.
32 Centers for Disease Control and Prevention (CDC). (2024). Signs and symptoms of untreated Lyme disease. Retrieved 7/22/2024.
33 Ziska, L., et al. (2016). Ch. 7: Food safety, nutrition, and distribution. The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 191.
34 Coleman-Jensen, A., et al. (2021). Household food security in the United States in 2020. ERR-298, U.S. Department of Agriculture, Economic Research Service, p. 9.
35 Ziska, L., et al. (2016). Ch. 7: Food safety, nutrition, and distribution. The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 195. doi.org/10.7930/J0ZP4417
36 Ibid, p. 195.
37 Ibid, p. 200. doi.org/10.7930/J0ZP4417
38 Coleman-Jensen, A., et al. (2021). Household food security in the United States in 2020. ERR-298, U.S. Department of Agriculture, Economic Research Service, p. 9.
39 Gamble, J.L., et al. (2016). Ch. 9: Populations of concern. In: The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, p. 255.
40 Ibid, p. 255.